Author: Anna Chou
Editors: Nicole Nwosu and Abidemi Oseni
Specialty: Autoimmune Disorder
Overview
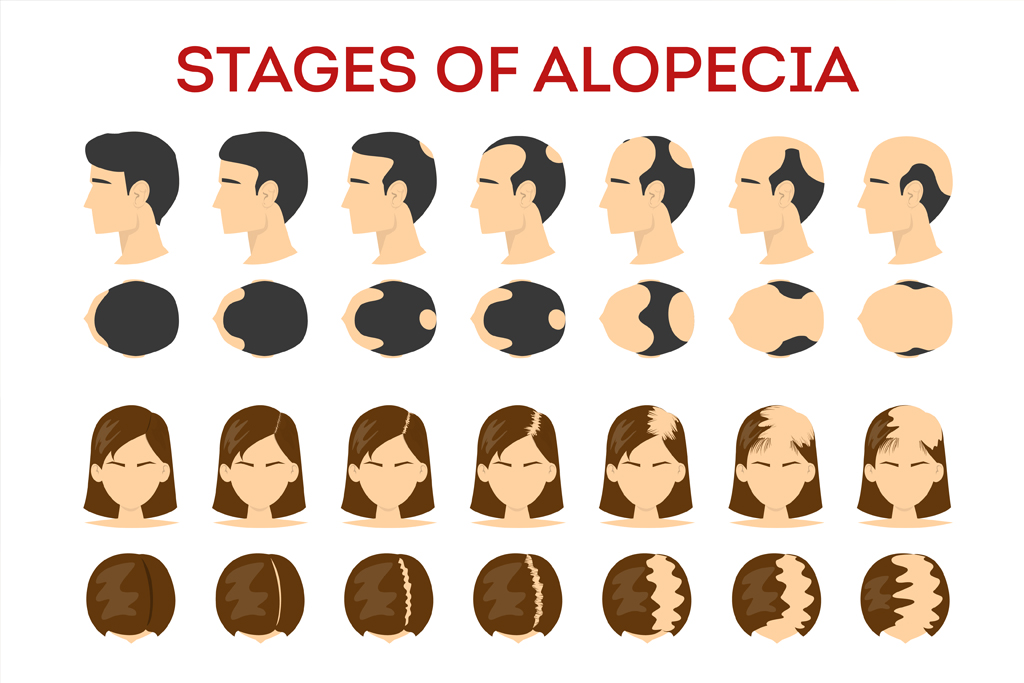
Alopecia areata is an autoimmune disease involving the hair follicle. This disease results in
chronic or acute patches of hair loss. In addition, the disease could lead to complete loss of hair
of the scalp, commonly known as alopecia totalis or complete hair loss of the entire body and
scalp which is known as alopecia universalis (Lai et al., 2019). Approximately 6 to 7million
members (2%) of the general population in the USA are affected by alopecia areata among both
children and adults, with genetic studies showing that the disease is polygenic (Pratt et al.,
2017)
Currently, the epidemiology, pathogenesis, and risk factors of alopecia areata are little
known or unknown when compared to other autoimmune diseases (Hordinsky, 2013)
Clinical manifestations alone are enough to help diagnose alopecia areata, although histopathologies
and dermoscopies can help with strengthening the diagnosis (Pratt et al., 2017).
What Causes Alopecia Areata?
Genetic associations between the immune system and alopecia areata have been studied and
established (Hordinsky, 2013). Apart from evidence of the disease being genetically contrived,
active alopecia areata can be characterized by bulb regions of anagen hair follicles being
surrounded by peribulbar lymphocytes (Hordinsky, 2013).
The expression of a natural killer group ligand is thought to attract killer (CD8+) T-cells to the bulb region, resulting in alopecia areata (Hordinsky, 2013). Additionally, a potential cause of alopecia areata is the collapse of
immune privilege in the hair follicle (Hordinsky, 2013).
Symptoms
Patients living with alopecia areata experience either complete hair loss on the scalp, and/or all
hair-bearing sites across the body (Hordinsky, 2013). As a result of the intrusive loss in part of
the integumentary system, patients are typically prone to sunburns, have hay fever or severe
allergic reactions due to loss of nasal hairs and have constant irritation in their unprotected eyes
due to dust and debris (Mendoza et al., 2013).
How Does My Doctor Know I Have Alopecia Areata?
Alopecia areata is a disease that can be diagnosed through clinical methods in the doctor’s
office, especially since the patients present with hallmark hair loss patterns (Wasserman et al.,
2007). Pathological methods that can aid in diagnosing the disease can be conducted via
dermoscopies and/or histopathologies (Pratt et al., 2017).
Patients suffering from alopecia areata may be susceptible to psychological distress such harassment and bullying in day to day life due to their appearances (Mendoza et al., 2013).
Treatment
There is currently no cure or therapy for alopecia areata. However, treatment options range
from topical, systemic and intralesional medications that depend on age, severity of the disease,
and secondary medical conditions (Hordinsky, 2013). The goal for treatment involves stopping
the progression of the disease and obtaining adequate hair growth (Lai et al., 2019). Trials for
therapeutic methods are underway for the condition but have yet to be approved (Hordinsky,
2013).
Articles on Misdiagnosis
Congenital temporal triangular alopecia. – Abstract—Europe PMC. (n.d.). Retrieved October 21,
2021, from https://europepmc.org/article/med/7285628
KoreaMed Synapse. (n.d.). Retrieved October 21, 2021, from
https://synapse.koreamed.org/articles/1063898
Trichostasis spinulosa misdiagnosed as alopecia areata—Goldust—2020—Dermatologic
Therapy—Wiley Online Library. (n.d.). Retrieved October 21, 2021, from
https://onlinelibrary.wiley.com/doi/abs/10.1111/dth.13513
Trichotillomania and Traction Alopecia | SpringerLink. (n.d.). Retrieved October 21, 2021, from
https://link.springer.com/chapter/10.1007/978-1-4471-4486-1_20
References
Hordinsky, M. K. (2013). Overview of Alopecia Areata. Journal of Investigative Dermatology
Symposium Proceedings, 16(1), S13–S15. https://doi.org/10.1038/jidsymp.2013.4
Lai, V. W. Y., Chen, G., Gin, D., & Sinclair, R. (2019). Systemic treatments for alopecia
areata: A systematic review. Australasian Journal of Dermatology, 60(1), e1–e13.
https://doi.org/10.1111/ajd.12913
Mendoza, T. R., Osei, J. S., Shi, Q., & Duvic, M. (2013). Development of the Alopecia
Areata Symptom Impact Scale. Journal of Investigative Dermatology Symposium
Proceedings, 16(1), S51–S52. https://doi.org/10.1038/jidsymp.2013.19
Pratt, C. H., King, L. E., Messenger, A. G., Christiano, A. M., & Sundberg, J. P. (2017).
Alopecia areata. Nature Reviews Disease Primers, 3(1), 1–17.
https://doi.org/10.1038/nrdp.2017.11
Wasserman, D., Guzman-Sanchez, D. A., Scott, K., & McMichael, A. (2007). Alopecia
areata. International Journal of Dermatology, 46(2), 121–131.
https://doi.org/10.1111/j.1365-4632.2007.03193.x