Specialty: Respiratory System, Pulmonology
Author: Praneesh Chandrasekhar
Editors: Shayan Mackie & Abidemi Oseni
Overview
Acute respiratory distress syndrome (ARDS) is a condition that disrupts the lungs ability to
successfully exchange gas. It is commonly associated with other conditions such as pneumonia and
represents a loss of functioning. Common symptoms are shortness of breath and lack of oxygen in the
body. Common risk factors have to do with poor quality of lungs and health through acts such as
smoking or alcohol as well as traumatic events or surgery.
Diagnosis of the condition is based on a ratio that measures the level of oxygen in the body as well as
a chest x-ray, however, these methods often lead to under or misdiagnosis of the condition due to lack
of clinical criteria to assess the condition as well as the specificity of presentation. Misdiagnosis also
has to do with the lack of reliability surrounding the current methods used to diagnose the condition as
many physicians have varied understandings of the results.
Treatment of the condition is primarily supportive, dealing with the symptoms at hand, so improving
oxygenation and breathing are main treatment outcomes. ARDS is also linked to COVID (Batah &
Fabro,2021).
What Causes Acute Respiratory Distress Syndrome?
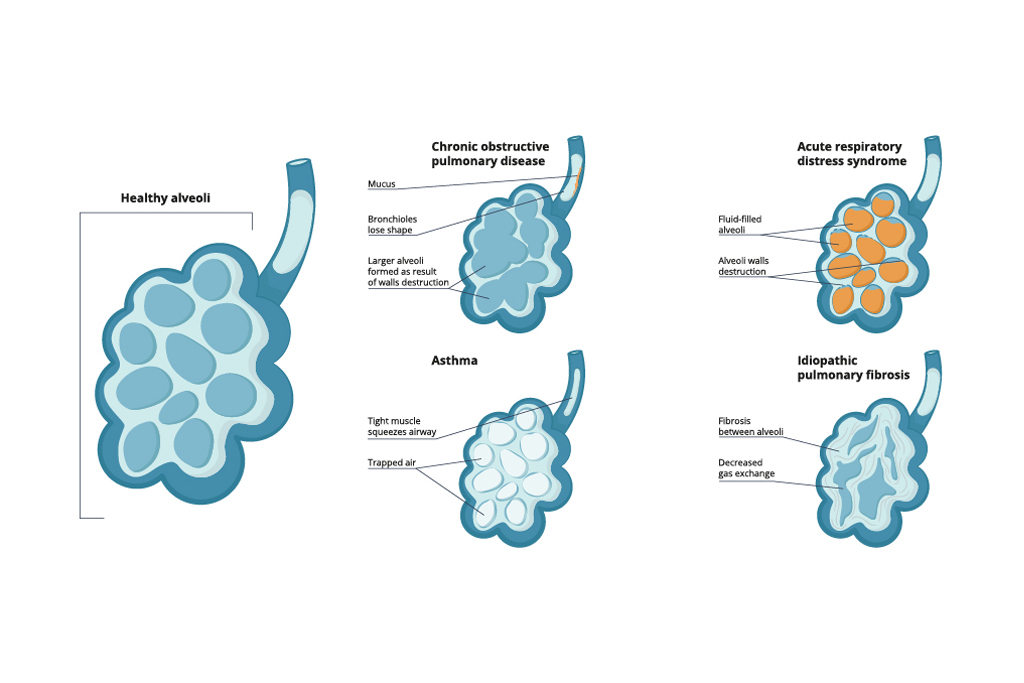
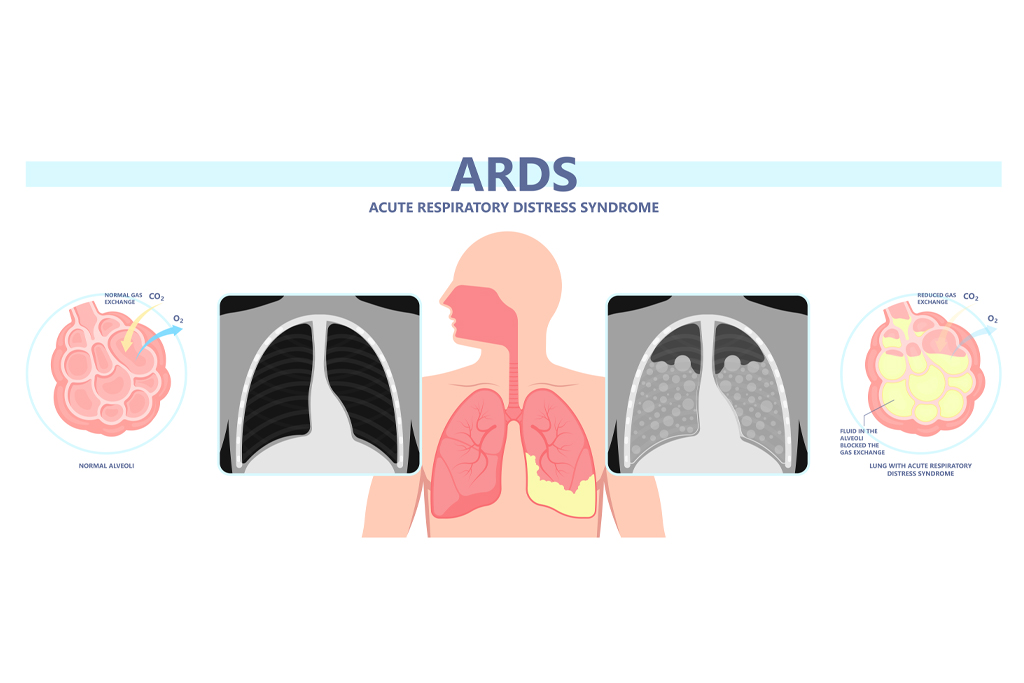
Acute Respiratory Distress Syndrome (ARDS) is a rapid onset condition that occurs in the smallest
part of the lungs known as the alveoli. Alveoli are single cell layer air sacs responsible for trading
oxygen and carbon dioxide to ensure the presence of oxygen in the bloodstream (Chaudhry &
Bordoni., 2021). Alveoli are covered with a network of blood vessels known as capillaries.
ARDS occurs when these air sacs become filled with fluid from these capillaries, an occurrence known as
non-cardiogenic pulmonary edema (Hupert, Matthay & Ware., 2019).
This damage to the alveoli can cause the alveoli to stop functioning altogether and lose its capacity to exchange carbon dioxide for oxygen (Hupert, Matthay & Ware., 2019).
Due to ARDS being a syndrome rather than a disease on its
own, it presents itself as a set of symptoms that are most often correlated to an already occurring
infection or condition.
Most commonly these conditions are:
● Pneumonia (viral or bacterial)
● Sepsis
● Food entering the windpipe
● Severe Trauma
(Matthay et al., 2019)
Symptoms
● Shortness of breath
● Lack of oxygen (Meyer, Gattinoni & Calfee, 2021)
Risk-Factors
● Advanced Age
● Female
● Smoking
● Alcohol Use
● Aortic Vascular surgery
● Cardiovascular surgery
● Traumatic Brain injury
● Hypoalbuminemia
● Long term exposure to ozone
● Vitamin D deficiency
(Diamond, Peniston, Sanghavi & Mahapatra et al., 2021) (Matthay et al., 2019) (Confalonieri, Salton,
Fabiano et al., 2017)
Medical Diagnosis
ARDS is diagnosed based on the Berlin definition of the syndrome. It quantifies 3 different severities
of the syndrome based on a particular ratio, Pao 2 /Fio 2 (Fan, Brodie & Slutsky, 2018). Pao 2 is a
measure of the pressure of oxygen currently present in the lungs measured in a common unit
describing pressure, mmHg (millimetre of mercury).
Fio 2 is a measure of the concentration of oxygen in the lungs, measured often as a fraction. Together, the ratio describes the relative oxygen levels of the patient. The Berlin definition quantifies these ratios into mild, moderate and severe levels of
ARDS:
● Mild: 200 mm Hg < Pao 2 /Fio 2 ≤ 300 mm Hg
● Moderate: 100 mm Hg < Pao 2 /Fio 2 ≤ 200 mm H
● Severe: Pao 2 /Fio 2 ≤ 100 mm Hg
(Fan, Brodie & Slutsky, 2018)
Diagnosis of ARDS also requires the use of a chest radiograph (CXR) to find “bilateral
interstitial and/or alveolar opacities consistent with pulmonary edema” (Kassirian, Taneja & Mehta,
2020). Essentially, this means the CXR can be used to look for scarring or scarred tissue in the lungs
that is caused by pulmonary edema.
ARDS has been consistently underdiagnosed. One reason being that the patient must display
very general symptoms in a very specific timeframe in order to be diagnosed with the condition
(Bellani, Pham & Laffey, 2020). Another reason is due to the lack of clinical testing available for the
condition. Although CXR and the Berlin definition exist, there are restrictions to their usage. CXR for
example has been said to be unreliable and have different understandings by different medical
professionals (Bellani, Pham & Laffey, 2020). The issue with the Berlin definition is due to different
measurements for the ratio mentioned earlier. The ratio is measured with a ventilator and often it does
not use standardised values, this leads to varying results that may show different Fio 2 values (Bellami,
Pham & Laffey, 2020). Due to these reasons, ARDS can often be underdiagnosed or misdiagnosed.
Some common conditions that are often confused with ARDS are listed below:
● Idiopathic acute interstitial pneumonia
● Hamman-Rich syndrome
● Acute exacerbation of idiopathic lung fibrosis
● Cryptogenic organising pneumonia
● Wegener granulomatosis
● Goodpasture syndrome
● Diffuse alveolar haemorrhage
● Acute hypersensitivity pneumonitis
● Acute hypereosinophilic pneumonia
(Aublanc, Perineal & Guérin, 2017)
Treatment
Treatment of ARDS is usually supportive through improving oxygenation and managing infections
and fluid levels. Improving oxygenation is preferably done through the use of non-invasive face
masks or helmets.
However, this non-invasive ventilation is only known to be useful for mild cases of
ARDS and is unclear in its effects on moderate to severe ARDS (Grieco et al., 2021). Non-invasive
respiratory support includes high flow nasal oxygen (HFNO), non-invasive ventilation (NIV), and
continuous positive airway pressure (CPAP) (Grieco et al., 2021).
HFNO heats and humidifies oxygen and directly delivers it to the nose using small insertions (Issa & Söderberg, 2021). NIV is a mechanical form of ventilation that uses either the lungs or surrounding muscles (abdomen or thorax) to cause air to enter the lungs (Scala & Pisani, 2018).
Continuous positive airway pressure is a technique that provides a constant flow of air to keep the lungs open (Rapelli et al, 2021).
A primary function of the non-invasive method is to try and get rid of the need for invasive
methods, otherwise known as, endotracheal intubation. Intubation is another technique designed to
provide oxygenation and ventilation, however, is often considered high risk.
In the case of ARDS, it has been shown that patients who had non-invasive methods done first and then later switched to intubation had a higher risk of mortality (Grieco et al., 2021). To learn more about treatment options
for ARDS, please refer to a healthcare professional for further guidance.
COVID-19
Considering that ARDS is a condition affecting the lungs, it has a strong connection to COVID-19. It
has been seen that some COVID patients are rapidly seeing ARDS as part of their condition (Batah &
Fabro, 2021). However, ARDS produces slightly different results when it is a part of COVID.
These patients are found to be developing lung fibrosis (thickening or extra scar tissue) along with normal
alveolar damage (Gibson, Quin & Pah, 2020). Patients are also seeing blood clots in the lungs due to
this condition (Gibson, Quin & Pah, 2020). Please note that receiving the COVID-19 vaccination is
strongly recommended by health professionals.
References
● Confalonieri, M., Salton, F., & Fabiano, F. (n.d.). Acute respiratory distress syndrome.
https://doi.org/10.1183/16000617.0116-2016
● Diamond, M., Feliciano, H. L. P., Sanghavi, D., & Mahapatra, S. (2021). Acute Respiratory
Distress Syndrome. StatsPearls[Internet]. https://www.ncbi.nlm.nih.gov/books/NBK436002/
● Matthay, M. A., Zemans, R. L., Zimmerman, G. A., Arabi, Y. M., Beitler, J. R., Mercat, A.,
Herridge, M., Randolph, A. G., & Calfee, C. S. (2019). Acute respiratory distress syndrome.
Nature Reviews Disease Primers 2019 5:1, 5(1), 1–22. https://doi.org/10.1038/s41572-019-
0069-0
● Aublanc, M., Perinel, S., & Guérin, C. (2017). Acute respiratory distress syndrome mimics:
The role of lung biopsy. Current Opinion in Critical Care, 23(1), 24–29.
https://doi.org/10.1097/MCC.0000000000000373
● Fan, E., Brodie, D., & Slutsky, A. S. (2018). Acute Respiratory Distress Syndrome: Advances
in Diagnosis and Treatment. JAMA, 319(7), 698–710.
https://doi.org/10.1001/JAMA.2017.21907
● Chaudhry, R., & Bordoni, B. (2021). Anatomy, Thorax, Lungs. StatPearls.
https://www.ncbi.nlm.nih.gov/books/NBK470197/
● Gibson, P. G., Qin, L., & Puah, S. H. (2020). COVID‐19 acute respiratory distress syndrome
(ARDS): clinical features and differences from typical pre‐COVID‐19 ARDS. The Medical
Journal of Australia, 213(2), 54-56.e1. https://doi.org/10.5694/MJA2.50674
● Kassirian, S., Taneja, R., & Mehta, S. (2020). Diagnosis and Management of Acute
Respiratory Distress Syndrome in a Time of COVID-19. Diagnostics 2020, Vol. 10, Page
1053, 10(12), 1053. https://doi.org/10.3390/DIAGNOSTICS10121053
● Issa, I., & Söderberg, M. (2021). High-flow nasal oxygen (HFNO) for patients with Covid-19
outside intensive care units. Respiratory Medicine, 187, 106554.
https://doi.org/10.1016/J.RMED.2021.106554
● Rapelli, G., Pietrabissa, G., Manzoni, G. M., Bastoni, I., Scarpina, F., Tovaglieri, I., Perger,
E., Garbarino, S., Fanari, P., Lombardi, C., & Castelnuovo, G. (2021). Improving CPAP
Adherence in Adults With Obstructive Sleep Apnea Syndrome: A Scoping Review of
Motivational Interventions. In Frontiers in Psychology (Vol. 12, p. 3266). Frontiers Media
S.A. https://doi.org/10.3389/fpsyg.2021.705364
● Bellani, G., Pham, T., & Laffey, J. G. (2020). Missed or delayed diagnosis of ARDS: a
common and serious problem. Intensive Care Medicine, 46(6), 1.
https://doi.org/10.1007/S00134-020-06035-0
● Scala, R., & Pisani, L. (n.d.). Noninvasive ventilation in acute respiratory failure: which
recipe for success? Number 3 in the Series “Highlights in acute respiratory failure” Edited by
Leo Heunks and Raffaele Scala. https://doi.org/10.1183/16000617.0029-2018
● Grieco, D. L., Maggiore, S. M., Roca, O., Spinelli, E., Patel, B. K., Thille, A. W., Barbas, C.
S. V., de Acilu, M. G., Cutuli, S. L., Bongiovanni, F., Amato, M., Frat, J. P., Mauri, T., Kress,
J. P., Mancebo, J., & Antonelli, M. (2021). Non-invasive ventilatory support and high-flow
nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS.
Intensive Care Medicine 2021 47:8, 47(8), 851–866. https://doi.org/10.1007/S00134-021-
06459-2
● Huppert, L. A., Matthay, M. A., & Ware, L. B. (2019). Pathogenesis of Acute Respiratory
Distress Syndrome. Seminars in Respiratory and Critical Care Medicine, 40(1), 31–39.
https://doi.org/10.1055/S-0039-1683996/ID/JR01437-42
● Batah, S. S., & Fabro, A. T. (2021). Pulmonary pathology of ARDS in COVID-19: A
pathological review for clinicians. Respiratory Medicine, 176, 106239.
https://doi.org/10.1016/J.RMED.2020.106239
● Meyer, N. J., Gattinoni, L., & Calfee, C. S. (2021). Seminar Acute respiratory distress
syndrome. Www.Thelancet.Com, 398, 2021. https://doi.org/10.1016/S0140-6736(21)00439-6
